by biomed | Jul 1, 2021 | News
What causes our bodies to age over time? One theory goes that it all begins at the cellular or even molecular level, where over time, damage to DNA in cells across the body accumulate and lead to mutation and cell senescence or death. In fact, it has been estimated that a single cell in the body can face up to hundreds of thousands of DNA lesions per day. Understanding where the DNA damage comes from, and how it is repaired, is key for improving our knowledge of how age-related diseases, including neurodegenerative disorders and cancer, originate.
“We were very surprised to find specific parts of the genome in neurons undergoing repeated DNA damage and repair. Previously, it was believed that damage occurred randomly across an individual cell’s DNA, but specifically in neurons we’ve now seen that there are special regions called enhancers that accumulate damage,” Will says. “These are very important regions of the genome that regulate how cells express their genes. It’s not hard to imagine how the damage we observe at these regions could, over time, lead to some of the effects of aging-related neurodegeneration.”
One key question remaining is where the DNA damage originates from. Will says the group believes it could be generated by the complicated process of turning on a gene, but future work will need to be done to clarify this. The collaborative study was supervised by Will’s mentor Dr. Andre Nussenzweig of the National Cancer Institute (NCI) and Dr. Michael Ward of the National Institute of Neurological Disorders and Stroke (NINDS), a fellow mentor of the NIH Oxford-Cambridge Scholars Program.
Will’s interest in the biological causes of aging began as summer research student in David Gius’ lab at Northwestern University. Dr. Gius, a former NIH Oxford-Cambridge Scholars Program Deputy Director, suggested Will consider the NIH Oxford-Cambridge Scholars Program for graduate school. After graduating from Middlebury College in 2016, Will joined the Program and has spent time between the University of Oxford, the National Cancer Institute, and the National Institute of Aging. In addition to his work on DNA repair in neurons, Will has another recent co-first author paper in Nature on identifying the “Achilles’ heel” of a class of specific cancers. After defending his thesis this summer, Will is staying on as a postdoc with Dr. Nussenzweig at NCI.

by biomed | Jun 9, 2021 | News
Why does SARS-CoV-2 infection cause devastating illness in some while others have only mild symptoms? A study published in Science last year found that neutralizing autoantibodies against IFNa and/or IFNw are the cause of a significant proportion of life-threatening COVID-19 cases. The study found that 13.7% of patients with critical COVID-19 had autoantibodies against IFNa and/or IFNw, while these autoantibodies were only detected in 0.3% of healthy individuals (samples collected prior to the COVID-19 pandemic).
“When identified early in the course of disease, detection of these autoantibodies could lead to novel therapeutic interventions, such as IFNb administration” said Lindsey Rosen, co-first author of the study. “We are hoping to screen samples collected from clinical trials where IFNb was used to treat COVID-19, some of which found a potential benefit of early IFNb administration. I hypothesize that some of the patients with positive outcomes have these autoantibodies and that exogenous IFNb helped them clear the virus more rapidly.”
Lindsey was recently recognized for her contributions to cytokine research as the first-place awardee of the 2020 William E. Paul Award. She will present her work and be recognized for her award at the upcoming NIH/FDA Cytokine Interest Group Mini Symposium on June 10, 2021, 10:00 am – 12:00 pm ET, on webex. Lindsey is currently finishing her doctoral research on autoimmunity at the University of Oxford and the National Institutes of Health as an NIH OxCam Scholar. After completing her DPhil, she plans to perform her postdoctoral research on anti-cytokine autoantibodies at the National Institutes of Health under the mentorship of Dr. Steve Holland.
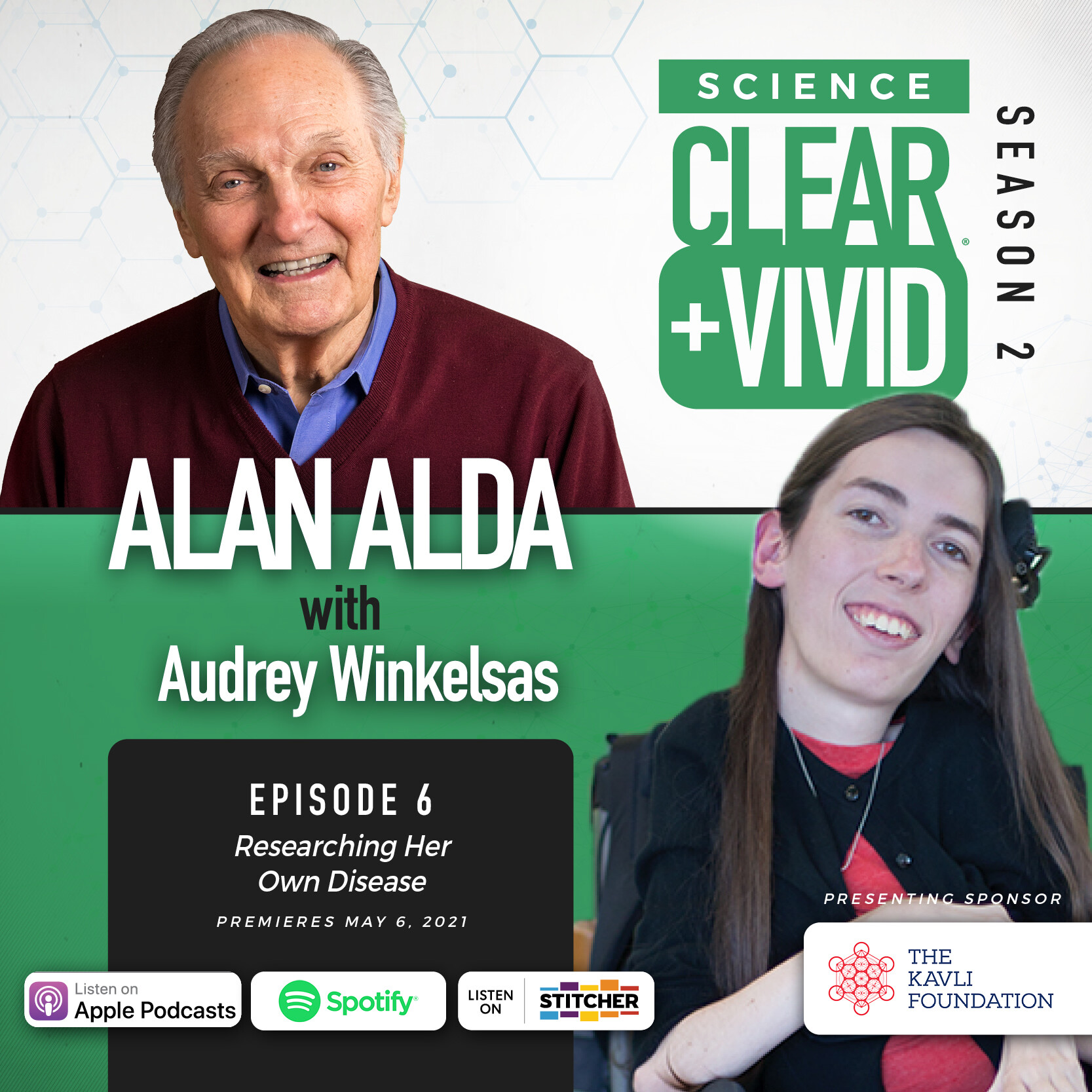
by biomed | May 6, 2021 | News
This week on Science Clear+Vivid host Alan Alda leads a conversation with another rising talent in science, Dr. Audrey Winkelsas. Dr. Winkelsas, an alumna of the NIH Oxford-Cambridge Scholars Program, recently completed her PhD work in the laboratories of Dr. Kenneth Fischbeck at the National Institute of Neurological Disorders and Stroke and Prof. Matthew Wood at the University of Oxford. During her PhD, Dr. Winkelsas investigated the molecular mechanisms in the pathogenesis of spinal muscular atrophy (SMA). She recently showed promising results for an RNA-targeting therapeutic developed to treat the debilitating genetic disease SMA.
Dr. Audrey Winkelsas has a rare genetic disease called Spinal Muscular Atrophy. While it limits her physical abilities, it has helped ignite her passion for science as she works at the laboratory bench – aided by her mother – to find a novel medication to help SMA patients manage the disease. Listen here.
“I am honored to have had the opportunity to talk with Mr. Alda! I hope that our conversation raises awareness about spinal muscular atrophy and the potential for RNA-based therapeutics to alter the course of many hereditary diseases. I also hope that our conversation communicates that people with disabilities, a group that is considerably underrepresented in science and medicine, have a place in these fields,” remarked Dr. Winkelsas.
Dr. Winkelsas will be attending the University of Michigan Medical School through Track 3 of the Medical Scientist Training Program this fall, furthering her goal of becoming a physician-scientist.
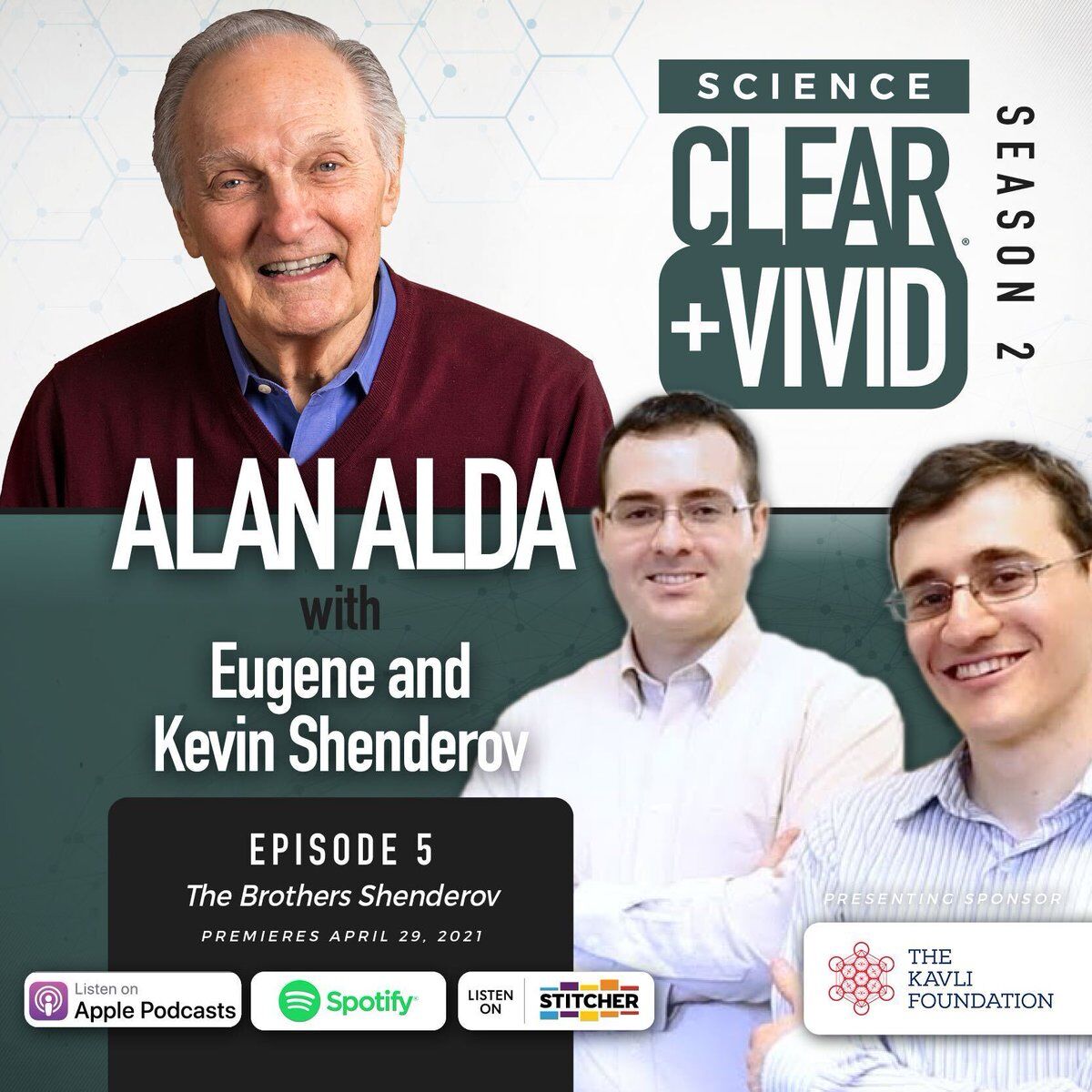
During this season’s podcast, Science Clear+Vivid host Alan Alda leads a conversation with 10 guests who each share their point of view and unique experience about basic science and their personal stories – what got them interested in or involved in science. Last week, Alan Alda spoke with physician-scientist brothers and NIH Oxford-Cambridge Scholars Program and Rhodes Scholars Alumni Dr. Eugene Shenderov and Dr. Kevin Shenderov. The “Brothers Shenderov” escaped with their parents from the Soviet Union shortly after being exposed to radiation from the Chernobyl disaster. They are now physician researchers whose personal experience shapes both their research and their relationship to their patients. Learn more and listen here.
by biomed | Apr 29, 2021 | News
You may recognize Emmy and Golden Globe Award winner Alan Alda from the hit series M*A*S*H and Scientific American Frontiers, but did you know he is a long-time science communication advocate? He is the founder of the Alan Alda Center for Communicating Science and is host of the hit podcast Science Clear+Vivid, supported by the Kavli Foundation.
Science Clear+Vivid features conversations with early career scientists on how curiosity is the engine of discovery and innovation and the power of basic scientific research – from the pure to the practical. What is curiosity-driven research? Why does it matter? How does it play a role in transforming our lives? Where does basic research take place, by whom and why is investing in basic research essential to society? Answering these deep-dive questions are among fuels the core mission of the International Biomedical Research Alliance and the graduate training program it enthusiastically supports – the NIH Oxford-Cambridge Scholars Program – so it is no wonder that three alumni of the program are included in Host Alan Alda’s interview line-up this season.
On the next episode of Science Clear+Vivid, released today, Thursday, April 29th, Alan Alda talks with two physician-scientist brothers, who are NIH Oxford-Cambridge Scholars Program Alumni and Rhodes Scholars – Dr. Eugene Shenderov and Dr. Kevin Shenderov. Brothers Eugene and Kevin Shenderov escaped with their parents from the Soviet Union shortly after being exposed to radiation from the Chernobyl explosion. They are now physician researchers whose personal experience shapes both their research and their relationship to their patients. Dr. Eugene Shenderov, Instructor of Oncology, and Dr. Kevin Shenderov, Instructor of Medicine, are both at Johns Hopkins Medicine.
Dr. Kevin Shenderov is currently a Chief Resident for the Johns Hopkins Hospital Internal Medicine residency program and will be returning to a Pulmonary/Critical Care Medicine fellowship in July. He aims to be a physician-scientist who helps develop novel therapies for critically ill patients with conditions such as sepsis and lung injury. “It was a pleasure to step away from the day to day of our current work in the hospital/lab to discuss the amazing advancements made possible by science (such as having a vaccine for COVID-19 within a year!) and the joy of the scientific process. I hope that budding scientists listening to the podcast will be encouraged to pick up their pipettes and start their own scientific journeys,” remarked Dr. Kevin Shenderov. In 2014, Johns Hopkins University highlighted The Brothers Shenderov: How a medical odyssey launched in the shadow of Chernobyl inspired the careers of two rising young stars in immunology.
On May 6, 2021, Alan Alda will talk with fellow NIH Oxford-Cambridge Aluma Dr. Audrey Winkelsas. Dr. Winkelsas graduated from Oxford University in 2020 and recently published a study focused on boosting levels of the protein missing in individuals with spinal muscular atrophy by interacting with specific RNA molecules. Learn more about her work here.
To stay up-to-date on Science Clear+Vivid, you can listen online, download it on Apple Podcasts or via your favorite streaming app.

by biomed | Apr 20, 2021 | News
A modified oncolytic herpes virus (oHSV) G207, alone and in combination with radiation, has been shown to be well tolerated with early signs of clinical effectiveness in pediatric patients with high-grade brain tumors finds a new study published in the New England Journal of Medicine earlier this month. “This is the first study utilizing a viral immunotherapy delivered directly into brain tumors in children. This work paves the way for an expanded Phase 2 and a litany of additional Phase 1 trials targeting unique pediatric CNS tumors and/or locations within the brain” says study coauthor Dr. Joshua Bernstock. “These results are truly exciting and represent a leap forward in the treatment of malignant pediatric brain tumors”. Dr. Bernstock was also co-first author on a new PLOS Biology paper published on April 7, 2021. This data provided the first evidence that NSCs (Neural stem cells) deliver functional mitochondria to target cells via EVs, paving the way for the development of novel (a)cellular approaches aimed at restoring mitochondrial dysfunction not only in multiple sclerosis, but also in degenerative neurological diseases.
Dr. Bernstock conducted his doctoral research on neuroprotection induced by certain classes of post-translational modifications at the University of Cambridge and the National Institutes of Health as an NIH OxCam Scholar. After completing his PhD, he went on to finish medical school at the University of Alabama at Birmingham were he also performed postdoctoral work examining the role of oHSVs as therapeutics in pediatric brain tumors under the mentorship of Dr. Gregory Friedman.
Dr. Bernstock is currently a neurosurgery resident at Brigham and Women’s and Boston Children’s Hospitals in Boston and intends to focus on pediatric neurosurgical oncology. A new parent himself, Dr. Bernstock said “I remain dedicated to translational science/medicine and it is my driving desire to improve outcomes for children with brain tumors by developing and improving novel, targeted therapies.”